PHIRST-C
About this project
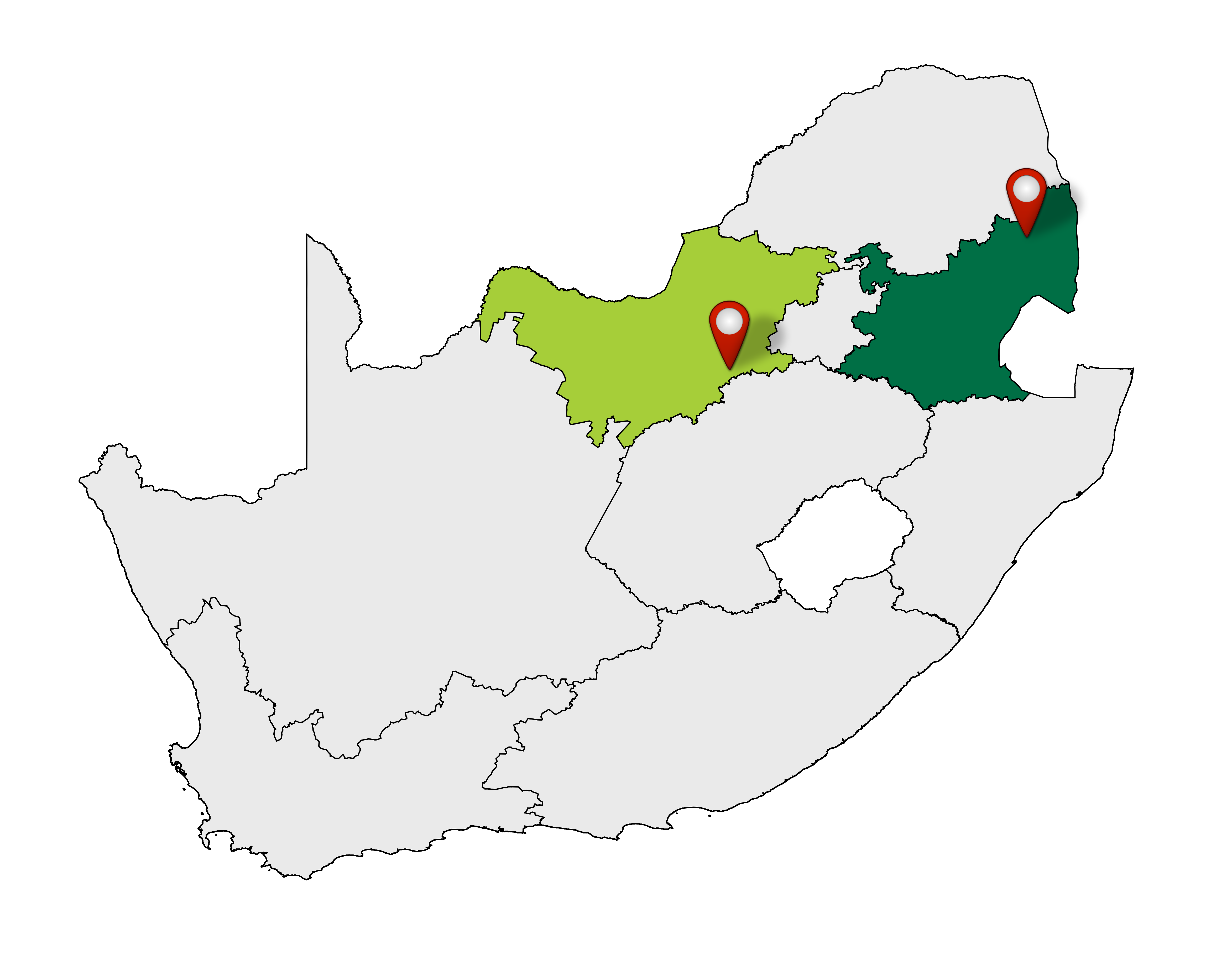
The Prospective Household study of SARS-CoV-2, Influenza, and Respiratory Syncytial virus community burden, Transmission dynamics and viral interaction in South Africa (the PHIRST-C Study) study builds on a previous study, the PHIRST study, that was implemented in 2016-2018 and focused on the community burden and household transmission of influenza, respiratory syncytial virus (RSV), Bordetella pertussis and pneumococcus. In light of the ongoing corona virus disease 2019 (COVID-19) pandemic, PHIRST-C will be conducted to help us understand the community burden, transmissibility potential and clinical features of illness associated with severe acute respiratory syndrome corona virus 2 (SARS-CoV-2) infection. PHIRST-C is a prospective household cohort study where we follow up 200 households, 100 in a rural community in Mpumalanga Province, and 100 in an urban community in the North West Province. Participants in the study are visited twice-weekly for from July 2020 – July 2021 to collect nasal swabs to test for SARS-CoV-2, influenza, RSV and pertussis; and to collect information on symptoms and healthcare seeking. Results will help us identify how many individuals are infected by SARS-CoV-2, how many of these experience symptoms, seek care, are hospitalised and die. Blood is collected every two months during this period to look for SARS-CoV-2 antibodies, signalling that someone was infected with the virus and their immune system reacted to that infection. To help us understand the reduction of antibodies in individuals that were infected, we will also be collecting blood every 2 months for an additional 6 months from participants who tested positive for SARS-CoV-2 in the initial follow-up period, helping us understand for how long someone may be immune to the virus after they were infected. Overall, PHIRST-C will help us understand who is more at risk for being infected with the virus and becoming severely ill, how long someone may stay infectious, if someone can be re-infected, what proportion of infections occur without any symptoms and to what extent individuals without symptoms can transmit the virus, how SARS-CoV-2 is influenced by other respiratory viruses such as influenza and RSV. We will also examine how age and HIV-infection affect all of the above areas. This information can then in turn be used to inform the design and duration of measures to contain the virus.
Objectives
- To estimate the community burden of SARS-CoV-2, including:
- the incidence of SARS-CoV-2 infection in the community as determined by polymerase chain reaction (PCR) and serologic assays;
- the correlation between individuals that seroconverted for SARS-CoV-2 and tested positive by PCR;
- the incubation period and the symptomatic fraction associated with SARS-CoV-2 infection;
- the spectrum of severity associated with symptomatic infections;
- the fraction of individuals with symptomatic infection seeking medical care; and
- the effect of the interaction of SARS-CoV-2 with influenza and RSV on disease severity.
- To assess the transmission dynamics of SARS-CoV-2 infections in the community, including:
- the estimation of the SARS-CoV-2 household secondary infection risk (SIR), generation time and length of shedding;
- the estimation of the probability of transmission of SARS-CoV-2 infection between individuals (both symptomatic and asymptomatic/presymptomatic) within the household and potentially the community;
- the estimation of the SARS-CoV-2 effective reproduction number (Rt) and its variation over time in the community; and
- the effect of the interaction of SARS-CoV-2 with influenza and RSV on transmission dynamics.
Impact
This study will provide essential information on the natural history of the virus that will impact decisions on optimal strategies for the containment and mitigation of the current and potential future epidemics of SARS-CoV-2 locally, regionally and globally.
Ethics
The study was approved by the University of the Witwatersrand Human Research Ethics Committee (Reference 150808) and the US Centers for Disease Control and Prevention relied on local clearance (IRB #6840).
Results
Gallery
Project Protocol
Funders and Collaborators
Sites